Click here to subscribe today or Login.
WILKES-BARRE — Gov. Tom Wolf and Acting Insurance Commissioner Jessica Altman recently said they are concerned the shortened enrollment period for the Affordable Care Act and reduced consumer outreach will have a negative impact on Pennsylvanians trying to sign up for coverage.
Ronald G. Ruman, director of communications at the Pennsylvania Insurance Department, said the open enrollment period this year has been shortened by the Trump Administration to Nov. 1 through Dec. 15, a reduction of about seven weeks from previous years.
Open enrollment starts Wednesday and ends Dec. 15 in most states, a sign-up period six weeks shorter than last year’s.
Some 9 million to 10 million people currently have private plans through the ACA’s government-sponsored markets. More than 8 in 10 receive subsidized premiums, and are cushioned from rate increases. Federal help paying premiums is still available despite GOP efforts to repeal the health law.
Ruman said the news is “particularly unfortunate” since the U.S. Census Bureau announced recently that Pennsylvania’s uninsured rate is down to 5.6 percent, the lowest on record, and down from 10.2 percent before the enactment of ACA.
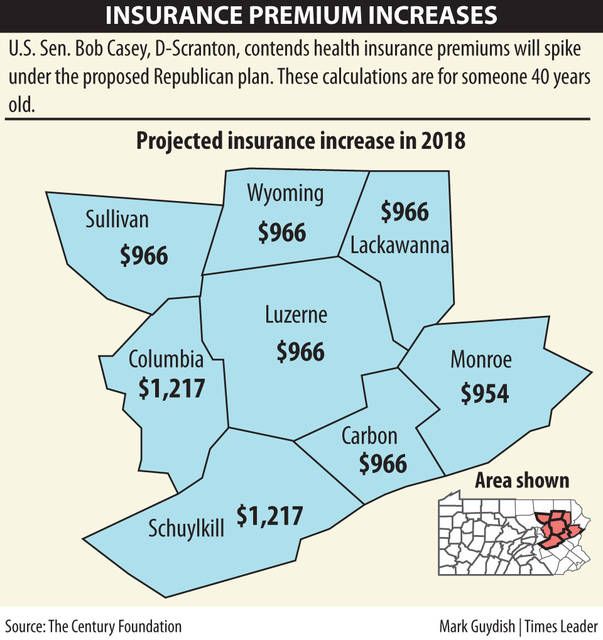
U.S. Sen. Bob Casey, D-Scranton, said this is another example of congressional Republicans and the Trump Administration sabotaging the nation’s health-care system.
“Northeastern Pennsylvanians will see increased premiums and higher costs because of this sabotage,” Casey said. “Instead of undermining our health-care system, the administration should be working in a bipartisan way to make it work better.”
According to information provided by U.S. Sen. Pat Toomey’s office, taken from the website healthcare.gov:
• The open enrollment period is the yearly period when people can enroll in a health insurance plan. The 2017 period started Nov. 1, 2016, and ended Jan. 31, 2017; the 2018 period runs in 2017 from Nov. 1 to Dec. 15.
• Outside the open enrollment period, you generally can enroll in a health insurance plan only if you qualify for a special enrollment period. You’re eligible if you have certain life events, such as getting married, having a baby, or losing other health coverage.
• Job-based plans might have different open enrollment periods. Check with your employer.
• You can apply and enroll in Medicaid or the Children’s Health Insurance Program (CHIP) any time of year.
An Associated Press story said many people already faced fewer choices and higher premiums. But President Donald Trump’s decision to cancel a subsidy to insurers that lowers consumer costs compounded the turmoil, pushing premiums even higher.
Add it all up and the number of uninsured people may start rising again, eroding gains that drove the uninsured rate to a historic low.
“It certainly is a hostile takeover,” said health policy expert Joe Antos of the right-leaning American Enterprise Institute in the AP story. “We are going to see a decline in enrollment. The people who will drop out in droves are the ones who are not getting a premium subsidy.”
Subsidized customers have a strong incentive to renew, but how many new people will join remains an open question. They’re vital because healthier, younger people are needed to keep rising premiums from destabilizing the marketplaces.
The AP story said already this year there was a big drop-off among consumers who buy individual coverage outside the government markets, and aren’t eligible for premium subsidies. Their costs, however, are generally tied to rising “Obamacare” rates. A recent analysis found premiums for popular silver plans rising an average of 34 percent next year. Monthly premiums can be as a high as a mortgage payment in some cases.
Polls show widespread consumer confusion — some are unsure if the health law has been repealed.
Trump administration officials say they’re aiming for smooth and efficient sign-ups. HealthCare.gov has new features intended to make it more user-friendly, and the call center is fully staffed.
Officials say they cut ads because spending so much money wasn’t warranted, and the scaled-back counseling programs weren’t enrolling many consumers. The programs take issue with that.